Hannah, a 13-year-old with nephrotic syndrome, appeared to be enjoying her teenage years as a great student and athlete. Beneath the surface, she had feelings of frustration and despair, as her medical condition showed no signs of improvement.
Hannah is not alone. Studies have shown chronic illnesses negatively impact children’s psychosocial well-being and increase their risk of anxiety and depression. Additionally, mental health screenings in primary care settings reveal substantial increases in anxiety and depression among patients with chronic illnesses.
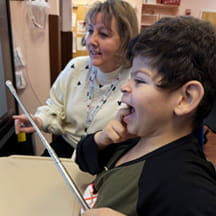
That’s why Atrium Health Levine Children’s Hospital implemented mental health screenings in their nephrology clinic.
“Primary care providers are recognized as intermediaries for mental health screenings and interventions, but as patients with chronic illness age, visits to their primary providers become less frequent and tend to be replaced with subspecialty visits,” said Susan Massengill, MD, director of pediatric nephrology and hypertension at Levine Children’s. “That more consistent visit schedule and the development of an ongoing healing relationship puts us in a unique position to identify and monitor those patients with mental health needs.”
Boosting mental health awareness
Levine Children’s aimed to increase recognition of anxiety and depression in pediatric nephrology patients over 12 years old using the validated GAD-7 and PHQ-9 screening tools. With support from the entire nephrology clinical care team and guidance from quality improvement coaches, Massengill and Laura Cary, LCSW, a nephrology social worker, began developing strategies to incorporate mental health screening into their existing workflow. The goal was 80% of eligible patients would be screened at their clinic visit and of those screened, 80% of patients with a score greater than or equal to five would receive an intervention.
To date, the team has sustained both the 80% screening and intervention goals. More than 2,400 screens have been completed and some 1,000 patients with elevated scores received individualized interventions and resources utilizing an innovative stepped intervention protocol developed by Cary. Upon rescreening, 64.5% had decreased GAD-7 anxiety scores and 61% had decreased PHQ-9 depression scores.
“Because we do these screens in real time and can recognize and intervene quickly, we think that is why we have such significant decreased scores and improved outcomes,” Massengill said.
Streamlining the process
Given the clinic’s high number of patients, Massengill and Cary opted for nurse-led screenings to initiate the process. From the start, the team prioritized staff education and support, collaborating with in-house psychologists, social workers, and quality improvement coaches to:
- Normalize mental health conversations.
- Practice scripting for in-person and virtual interactions.
- Provide nurses with a job aid outlining how to document scores and interventions within the patient’s electronic medical record.
“It was critical that nurses felt comfortable with their understanding of pediatric depression and anxiety and had the tools needed to successfully carry out this process,” Cary said.
To improve the screening process, the nephrology team worked with data scientists to create an automated pre-visit planning (PVP) report emailed daily to the clinical team. The report identifies which patients are due for a screen and lists previous screening scores for reference. This process allows the nurses and social workers to anticipate patient screening needs ahead of the following day’s clinic. Referencing the PVP report, the nurses welcome and room the patient, and then offer the two-minute paper screening. Completed screening scores are documented in the electronic medical record during the patient’s visit and the intervention protocol is initiated when applicable.
Determining the root cause
To better individualize interventions, the team also sought to understand the root causes of the patients’ anxiety. Three additional questions were added to the original GAD-7 screening asking specific questions to assess whether the patient’s feelings of anxiety stemmed from their medical diagnosis, social and environmental factors, and/or from upcoming procedures or lab draws.
“This feedback was essential to tailoring interventions specific to the patient’s need and having more focused and intentional conversations” Cary said.
Integrating interventions and rescreens
Cary worked with a multidisciplinary team to develop a stepped intervention protocol for anxiety and depression. Patients scoring in the mild range (5-9) received informational resource handouts, while those scoring 10 or greater on the screening tool were immediately referred to a social worker. An extension to the intervention protocol was added specifically for patients who exhibited suicidal ideation on their depression screen.
“This protocol was instrumental in increasing staff comfort and confidence around anxiety and depression and how to handle situations where screening scores were elevated,” Cary said. “It also helped establish a more efficient screening and intervening workflow.”
Patients with scores greater than five are rescreened every three months while those with scores less than five are screened annually or sooner if requested by a patient, the patient’s family, or a provider. Patients with persistent mild anxiety are referred to a social worker for further support.
Spreading the conversation
As the team looks ahead, Massengill and Cary hope to partner with primary care providers to coordinate follow-up interventions for patients who do not return to the nephrology clinic within the three-month rescreening timeframe. Additionally, they want to explore opportunities to address mental health in patients younger than 12 and focus on the emotional well-being of the patient’s family and caregivers as well. Hospital-wide efforts to engage providers in mental health conversations are in the works and a mental health screening change package will be shared with other specialties.
“We hope to highlight the importance of mental health screenings and help other hospitals incorporate screenings and interventions into an existing subspecialty clinic workflow,” Massengill said. “We know how important it is to be able to intervene early in these situations and have seen the positive impact it can have.”